Risk of Untreated Sleep Apnea
What is Sleep Apnea?
Obstructive Sleep Apnea is a common but serious sleep disorder. The disorder is caused by repetitive periods when airflow is interrupted during sleep due to a narrowing or closure to the throat. A complete blockage of airflow is an apnea, and a partial interruption is a hypopnea. Each apnea or hypopnea can result in drops in oxygen levels and brief awakenings or sleep disturbances.
The disorder can stress your heart and other organs due to the recurrent drops in oxygen levels, which can cause abnormalities in blood pressure, levels of hormones, inflammation, and other changes.
Untreated sleep apnea may increase the risk of motor vehicle crashes or work-related accidents, poor control of blood pressure, diabetes, heart disease, stroke, and liver problems.


Sleep Apnea Statistics
Type II Diabetes
Sleep Apnea is seen in 58% of patients with Type II diabetes
Atrial Fibrillation
Patients with Obstructive Sleep Apnea have a 4 times greater risk of AFIB
Motor Vehicle Accident
Patients with sleep apnea were nearly 2.5 times more likely to be the driver in a motor vehicle accident.
Cardiovascular Disease
Patients with untreated severe OSA were more likely to die of cardiovascular disease





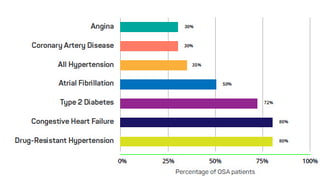
Prevalence of OSA in patients with co-morbid conditions

What if I don't treat my Sleep Apnea?
Heart Implications
Much research has shown that OSA takes a heavy toll on the heart. In 2021, the American Heart Association (AHA) issued a scientific statement emphasizing how sleep apnea worsens heart disease, and why increased awareness on the part of physicians and patients is so important. Among the highlights:
Between 40% and 80% of people in the US with cardiovascular disease also have OSA, yet it is underrecognized and undertreated by doctors.
In general, about 34% of middle-aged men and 17% of middle-aged women meet the criteria for OSA.
Sleep apnea can cause a negative feedback loop whereby it worsens cardiovascular conditions, which in turn worsen sleep apnea.
OSA affects 30% to 50% of people with high blood pressure and is a risk factor for atrial fibrillation.
OSA is also associated with Type 2 diabetes, worse outcomes from heart failure, and even sudden cardiac death.
People with cardiovascular risk factors or conditions should be screened for OSA, and treated appropriately. This may include continuous positive airway pressure (CPAP), oral appliances, modifying lifestyle behaviors and weight loss.
Risk factors for OSA include obesity, large neck circumference, craniofacial abnormalities, smoking, family history, and nighttime nasal congestion.
OSA is associated with several cardiovascular complications, as detailed in the statement:
High blood pressure – OSA is present in 30%-50% of people with high blood pressure, and up to 80% of those who have resistant, or hard-to-treat high blood pressure;
Heart rhythm disorders such as atrial fibrillation and sudden cardiac death;
Stroke;
Worsening heart failure;
Worsening coronary artery disease and risk of heart attack;
Pulmonary hypertension (PH) – as many as 80% of people with PH have OSA; and
Metabolic syndrome and Type 2 diabetes.
The good news is, treating OSA can improve heart problems and help prevent them. Talk with your doctor about these suggestions from the AHA statement authors:
If you are diagnosed with OSA, get treated with available therapies, potentially including lifestyle and behavior modifications and weight loss.
If you have severe OSA, get treated with a CPAP device when possible.
If you have mild-to-moderate OSA, get treated with oral appliances that adjust the jaw and tongue placement during sleep to prevent obstructed breathing.
Have routine follow-up, including overnight sleep testing to confirm if treatment is effective.
Other OSA Consequences
OSA does not just affect the heart. Research shows connections with:
Memory and cognition. A number of studies connect OSA with cognitive problems and memory loss. One recent study found that OSA interferes with your ability to recall specific details of events that happened in your own life. The authors discovered that brain scans of people with OSA showed a significant loss of grey matter in the brain in regions that overlap with biographical memory.
Brain damage. According to the American Academy of Sleep Medicine, the breathing pauses that occur during OSA can prevent your body from supplying enough oxygen to the brain. In severe cases, this can lead to a significant reduction in the brain’s white matter, leading to difficulty concentrating and moodiness, as well as memory problems. However, the damage was reversible with CPAP therapy.
Asthma. A recent review article revealed that undiagnosed or inadequately treated OSA adversely affects asthma control, and that asthma and the medications that treat it predispose to OSA.
Weaker bones and teeth. A recent study has found a connection between sleep apnea and low bone-mineral density, suggesting that OSA can lead to increased fractures, loose teeth and failed dental implants.
Road traffic accidents. The first nationwide study to estimate the risk of all road traffic accidents in individuals with OSA was conducted using data from Denmark. The researchers found the risk of having a motor vehicle accident was significantly higher among those with OSA and that accidents were more severe among those with OSA compared with similar individuals who did not have OSA. That study also found that OSA did not increase the risk of pedestrian or biking accidents.




What therapy will you choose?
Be kind and help others who are trying to choose a therapy by answering 5 quick questions about your decision.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are intended for educational purposes only.
No content or material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding your medical condition.
Reliance on any information provided on this website is solely at your own risk.